Posted on January 19th, 2016
Brian
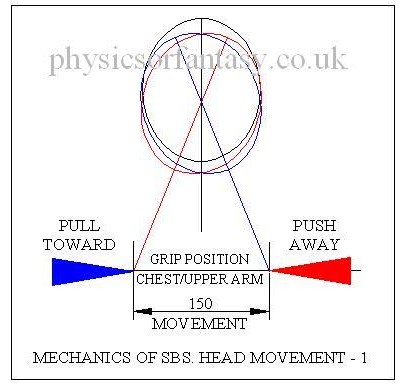
The following drawing shows the basic mechanics relating to shaking a baby. Surprisingly, the total shaking movement of the child’s body, to and fro, is only about 6″ (150mm). Just try it and see, (but not on a real child, please) and you will find it difficult and uncomfortable to make it more than that. You should also realise that it’s the child’s body that is shaken, not it’s head.
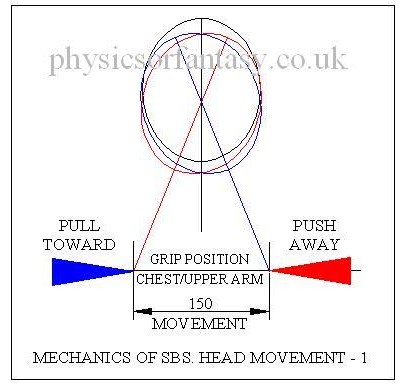
As the head is not rigidly fixed to the body it does not move this same 6″ but moves up and down by a few millimetres and also rotates by about 20º each side of the vertical, the neck bending to allow this to happen. There are only small acceleration forces acting on the head. Basically, the body moves relative to an almost stationary head
The inertia of the child’s head restricts any rapid movements to it. Any movements of the head can only be caused by forces acting through the neck, which is very flexible. Any serious movements to the head would cause serious damage to the spine which is just as fragile as the brain.
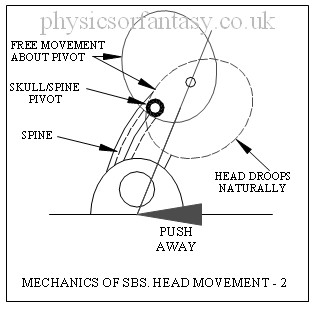
The following drawing refers to the auxiliary head movements that should also be considered.
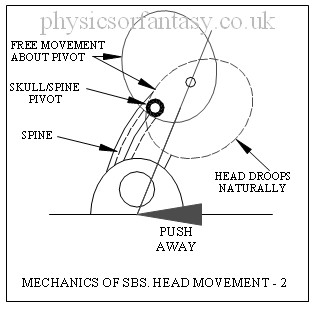
The relatively free ‘nodding’ movement of the head is entirely consciously controlled by muscles in the neck. If you fall asleep your head will freely fall backwards, sideways or forward. Undue accelerations in this movement would likely cause neck muscle and tendon damage plus damage to the complex pivot assembly because in the SBS case the child is assumed to be awake. However, these same injuries could also happen during the birth process.
I sent data to the Louise Woodward defence team relating to the mechanics of Shaken Baby Syndrome in 1997.
Anyone who watched the case on television, after the defence team brought in a specialist engineer, must have been amazed by the prosecution attorney’s ridiculous antics whilst attempting to show how the head could be held in such a way that it was shaken along with the body. She had obviously spent a lot of time thinking about this, but the contortions she got into made it obvious that Louise Woodward could never have carried out the same rigmarole in a fit of anger.
———————————–
Abstract.
Dynamic Biomechanical Findings on Shaken Baby Syndrome/Lethal Minor Falls
http://sbsreferences.com/DownloadHandler.ashx?pg=392f9051-f6fa-4a54-a2d8-70157cf253c0§ion=11dab90f-171c-4263-9334-b175c406f533&file=Exhibit+14A.pdf
FROM: Injury Biomechanics Researcher: Chris Van Ee, PhD
TO: The Honorable Court
SUBJECT: Dynamic Biomechanical Findings on SBS-LMF
DATE: March 3, 2008
Dynamic Biomechanical Findings March 7, 2008 Page 2 of 4
2. SBS/LMF Findings From Biomechanical Tests and Studies:
(A) Scientific testing has shown that head acceleration levels from anterior/posterior human shaking of a normal 0- to 2-year-old child in the sagittal plane results in head acceleration and force levels that are much lower than those which are associated with traumatic head injury. Repeated testing of this hypothetical has shown that the head accelerations associated with shaking are far below the level associated with injury and there is no quality data to support the SBS brain injury mechanism. Thus shaking, even if done in a fit of anger, is not expected to result in head dynamics sufficient to cause direct intracerebral trauma.
(B) Human shaking (id.) may cause lethal brain stem and cervical spine injuries in a 0-to 2-year-old child, as the forces necessary for these injuries are well below the level needed for fatal brain injuries and are consistent with the forces that can be produced in shaking. Put another way, these neck injuries would be expected in any hypothetical-superhuman-strength case of SBS where superhuman dynamics resulted in head accelerations leading to intercerebral trauma (if SBS were valid, which it is not).
————————————–
Abstract from
Shaken baby syndrome: A biomechanics analysis of injury mechanisms.
Traumatic infant shaking has been associated with the shaken baby syndrome (SBS) diagnosis without verification of the operative mechanisms of injury. Intensities for SBS have been expressed only in qualitative, unsubstantiated terms usually referring to acceleration/deceleration rotational injury and relating to falls from great heights onto hard surfaces or from severe motor vehicle crashes. We conducted an injury biomechanics analysis of the reported SBS levels of rotational velocity and acceleration of the head for their injury effects on the infant head-neck. Resulting forces were compared with experimental data on the structural failure limits of the cervical spine in several animal models as well as human neonate cadaver models. We have determined that an infant head subjected to the levels of rotational velocity and acceleration called for in the SBS literature, would experience forces on the infant neck far exceeding the limits for structural failure of the cervical spine. Furthermore, shaking cervical spine injury can occur at much lower levels of head velocity and acceleration than those reported for the SBS. These findings are consistent with the physical laws of injury biomechanics as well as our collective understanding of the fragile infant cervical spine from (1) clinical obstetric experience, (2) automotive medicine and crash safety experience, and (3) common parental experience. The findings are not, however, consistent with the current clinical SBS experience and are in stark contradiction with the reported rarity of cervical spine injury in children diagnosed with SBS. In light of the implications of these findings on child protection and their social and medico-legal significance, a re-evaluation of the current diagnostic criteria for the SBS and its application is suggested.
Faris A. Bandak. Department of Neurology, A1036 F. Edward Hébert School of Medicine, Uniformed Services, University of the Health Sciences, Bethesda, MD 20814, USA
—————————-
Abstract from Wikapedia/cheshire nanny case (Louise Woodward Trial. 1967)
Patrick Barnes, a pediatric radiologist at Stanford University, was a key prosecution witness in the trial, but in 2011 said he would not give the same testimony today. He said there had been a revolution in the understanding of head injuries in the past decade, partly due to advances in MRI brain scanning technology: “We started realizing there were a number of medical conditions that can affect a baby’s brain and look like the findings that we used to attribute to shaken baby syndrome or child abuse”, such as infections and in utero strokes.
—————————-
MORE TO FOLLOW SHORTLY.
Author – Brian Williams
Read also; Shaken Baby Syndrome-Debunking the Myth
Shaken baby syndrome: A biomechanics analysis of injury mechanisms
Posted on January 2nd, 2016
Brian
Birth Brain Injuries
1. What is a ‘normal’ birth?
Figures given in ‘ESSENTIAL OBSTETRICS & GYNAECOLOGY’ (E.O.G.) Chapter 17, indicate that 6.7% of live births in England & Wales are Low Birth Weight i.e. less than 2.5 kilograms.
From the same chapter we are told that the common causes of death in the 1st 4 weeks of life are;
1. Major congenital abnormalities incompatible with life.
2. Prematurity- the most important single factor in causing neonatal death, associated with,
a. Respiratory Distress Syndrome.
b. Pnuemonia.
c. Intercranial Haemorrhage and cerebral damage sustained either during labour and delivery or in the early neonatal period.
d. Necrotizing enterocolitus.
From NEONATAL NEUROLOGY page 139, we are told that ” Levene and Starte (1981) studied 202 consecutive admissions of all birth weights, 68 (34%) of whom were found to have intracranial haemorrhage”
From NEONATAL NEUROLOGY page 76, we are told that approx. 27% of premature infants born in the 31st to 34th weeks develop Periventricular haemorrhages.
From NEONATAL NEUROLOGY ,page 63, we are told that approx. 7% of premature infants born with a birth weight of 1.8 kilograms or less have subarachnoid haemorrhage.
From NEONATAL NEUROLOGY page 57, we are told that ” Intracranial haemorrhage occurs commonly in newborn infants and is an important cause of death & handicap.”
It is evident therefore, that brain haemorrhages in infants is common.
It is also a well documented fact that due to the lack of development of the blood vessels the premature infant is at an increased risk of haemorrhage.
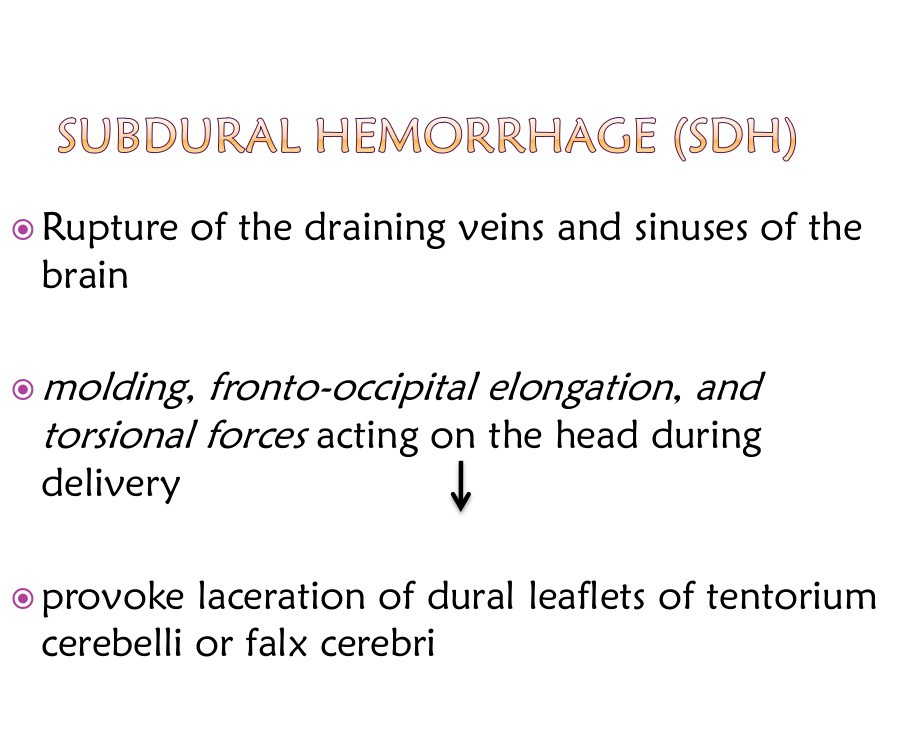
Subdural Haematomas.
From NEONATAL NEUROLOGY, page 58, we are told that “the cause of this type of condition is usually traumatic, that the incidence of it has greatly reduced over recent years and that It has not however, completely disappeared; indeed it may still be a relatively common lesion affecting the neonatal brain and may be associated with few clinical signs, thus remaining undiagnosed during life.”
I need to tidy up the following two graphics and information on originators. Brian.
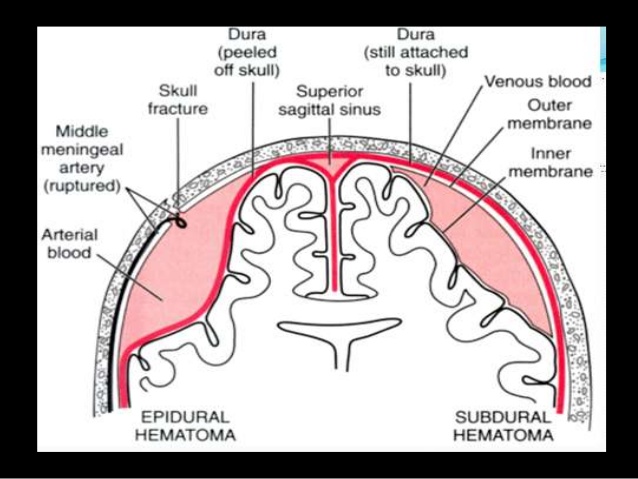
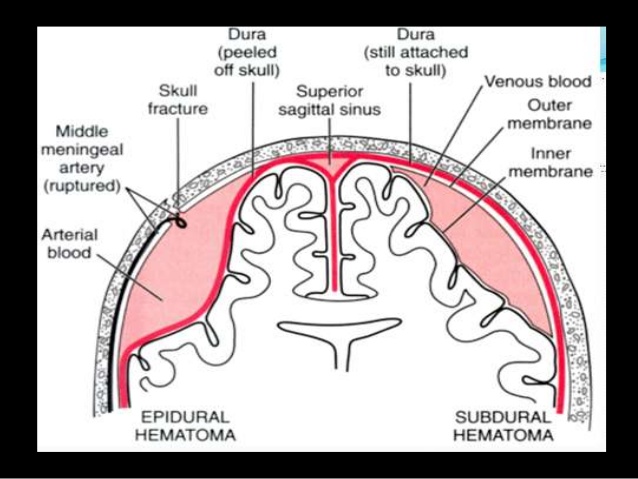
Intracranial Haemorrhages
Note the difference between the following two sets of statements referring to the cause of subdural haemorrhages.
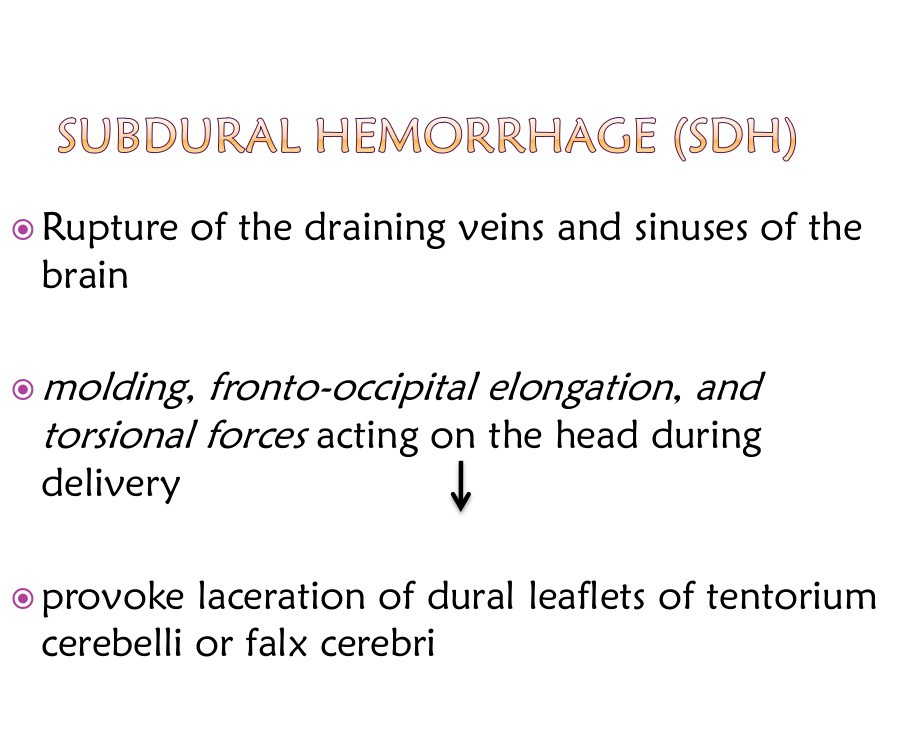
 The first is a bit confusing (like most medical literature) but I read this as 1. Actual damage to the head. 2. Caused by distortion of the brain during the birth process.
The first is a bit confusing (like most medical literature) but I read this as 1. Actual damage to the head. 2. Caused by distortion of the brain during the birth process.
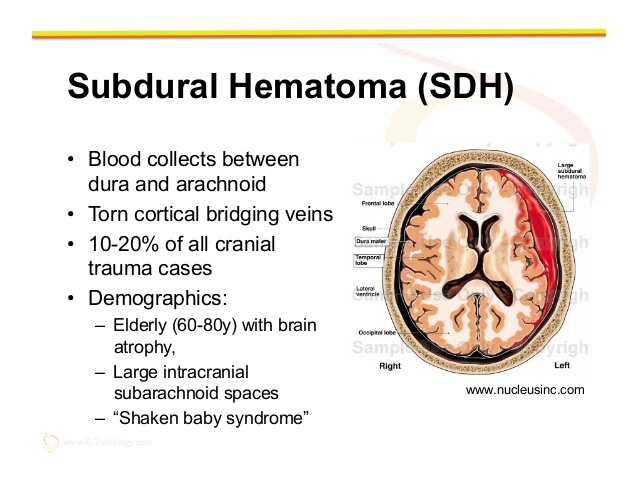
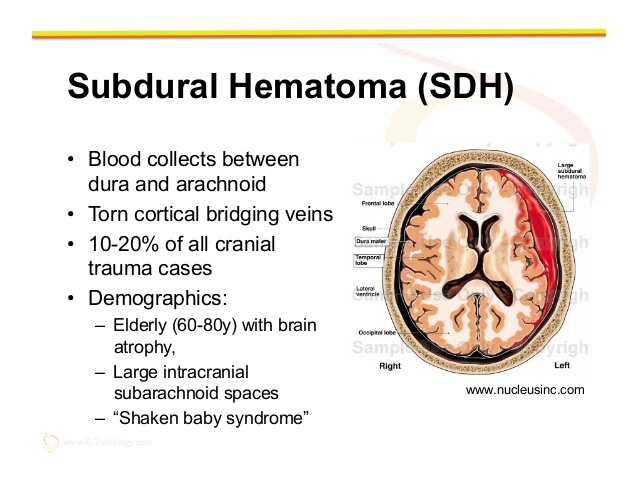
The second set of statements is also slightly confusing, but I read this as “Blood collects between the dura and arachnoid layers, due to torn veins. Subdural Haematomas comprise 10 – 20% of all cranial trauma cases.
The three main causes of the torn veins is 1. Brain atrophy in the elderly. 2. Large intracranial subarachnoid spaces.
3. “Shaken Baby Syndrome”.
Relating to demographics, it should read. 1. Elderly people with brain atrophy. 2. People with large intracranial subarachnoid spaces. 3. “Shaken Baby Syndrome” is not a demographic type.
There can be many causes of subdural haemotomas to people who are not between the ages of 60-80 with brain atrophy, or people who have large intracranial subarachnoid spaces.
Falls can occur to people of all ages. Are the paediatricians really asking us to believe, that subdural Haematomas only happen to the people mentioned in the above two demographic categories plus babies that are shaken or thrown about? If a 30year old man falls off a ladder, are the paediatricians saying that the man cannot suffer from a subdural Haematomas due to falling?
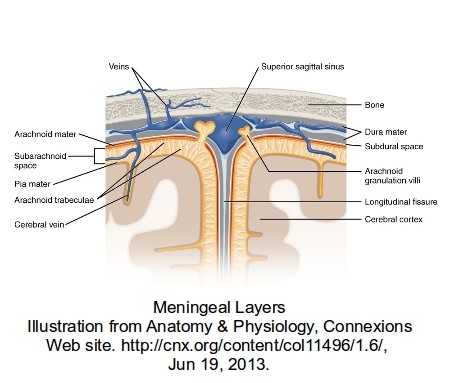
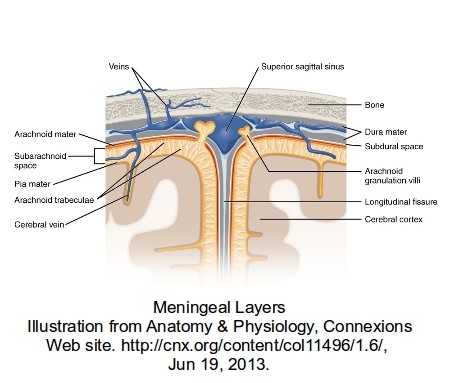
In the drawing below there are numerous large and small veins shown. During the birth process the head can get quite seriously distorted, because at this stage the skull is quite soft and pliable to enable the head to pass through the birth canal.
 Excluding any accelerations or decelerations (obviously not applicable during the birth process unless the paediatrician is (non-accidentally) shaking the mother or throwing her onto the floor), the main stresses are distortions to the head caused primarily by the natural pressure of the birth process working against the restriction of the birth canal. It should be remembered that the skull is not bone at this stage, and although giving some protection to the brain, is not a crash helmet. In the area of the fontanelle, the very soft area of the skull in babies, the brain is virtually unprotected.
Excluding any accelerations or decelerations (obviously not applicable during the birth process unless the paediatrician is (non-accidentally) shaking the mother or throwing her onto the floor), the main stresses are distortions to the head caused primarily by the natural pressure of the birth process working against the restriction of the birth canal. It should be remembered that the skull is not bone at this stage, and although giving some protection to the brain, is not a crash helmet. In the area of the fontanelle, the very soft area of the skull in babies, the brain is virtually unprotected.
Squeezing of the brain tends to to force it forward and bulge into the fontanelle area, but being restrained by the dura-mater. This will cause stretching on the inside of the dura-mater that can damage veins and capillaries that then bleed into the subdural space.
Obviously there are many things to consider; Is it a rapid/easy birth or an extended/complicated birth? Is it a full term baby or premature? How much external handling of the birth was required?
The birth process is not a guaranteed simple process especially in a first birth for the mother. The mother’s natural anxiety with her first birth can complicate the process. The mother’s anatomy can have a great effect on the birth process.
Jaundice Causes
By Mayo Clinic Staff
Excess bilirubin (hyperbilirubinemia) is the main cause of jaundice. Bilirubin, which is responsible for the yellow color of jaundice, is a normal part of the pigment released from the breakdown of “used” red blood cells.
Normally, the liver filters bilirubin from the bloodstream and releases it into the intestinal tract. A newborn’s immature liver often can’t remove bilirubin quickly enough, causing an excess of bilirubin. Jaundice due to these normal newborn conditions is called physiologic jaundice, and it typically appears on the second or third day of life.
Other causes
An underlying disorder may cause jaundice. In these cases, jaundice often appears much earlier or much later than physiologic jaundice. Diseases or conditions that can cause jaundice include:
-
Internal bleeding (hemorrhage)
-
An infection in your baby’s blood (sepsis)
-
Other viral or bacterial infections
-
An incompatibility between the mother’s blood and the baby’s blood
-
A liver malfunction
-
An enzyme deficiency
-
An abnormality of your baby’s red blood cells that causes them to break
—————————————
From. wikipedia.org/wiki/Shaken_baby_syndrome/legal issues
In 2012, Dr. A. Norman Guthkelch, the neurosurgeon often credited with “discovering” the diagnosis of SBS,[54] published an article “after 40 years of consideration,” which is harshly critical of shaken baby prosecutions based solely on the triad of injuries.[55] Again, in 2012, Dr. Guthkelch stated in an interview, “I think we need to go back to the drawing board and make a more thorough assessment of these fatal cases, and I am going to bet . . . that we are going to find in every – or at least the large majority of cases, the child had another severe illness of some sort which was missed until too late.”[56] Furthermore, in 2015, Dr. Guthkelch went so far as to say, “I was against defining this thing as a syndrome in the first instance. To go on and say every time you see it, it’s a crime…It became an easy way to go into jail.”[57]
On the other hand, Teri Covington, who runs the National Center for Child Death Review Policy and Practice, worries that such caution has led to a growing number of cases of child abuse in which the abuser is not punished.[54]
This is a rather nasty statement (by Teri Covington) to make. She is implying that irrespective of the evidence, the people charged with SBS are actually the abusers. Brian.
———————————–
More to follow
——————————————
Author; Brian Williams.